- Like
- Digg
- Del
- Tumblr
- VKontakte
- Buffer
- Love This
- Odnoklassniki
- Meneame
- Blogger
- Amazon
- Yahoo Mail
- Gmail
- AOL
- Newsvine
- HackerNews
- Evernote
- MySpace
- Mail.ru
- Viadeo
- Line
- Comments
- Yummly
- SMS
- Viber
- Telegram
- Subscribe
- Skype
- Facebook Messenger
- Kakao
- LiveJournal
- Yammer
- Edgar
- Fintel
- Mix
- Instapaper
- Copy Link
By Eve Marcum-Atkinson, WV CAG’s Director of Healthcare Advocacy
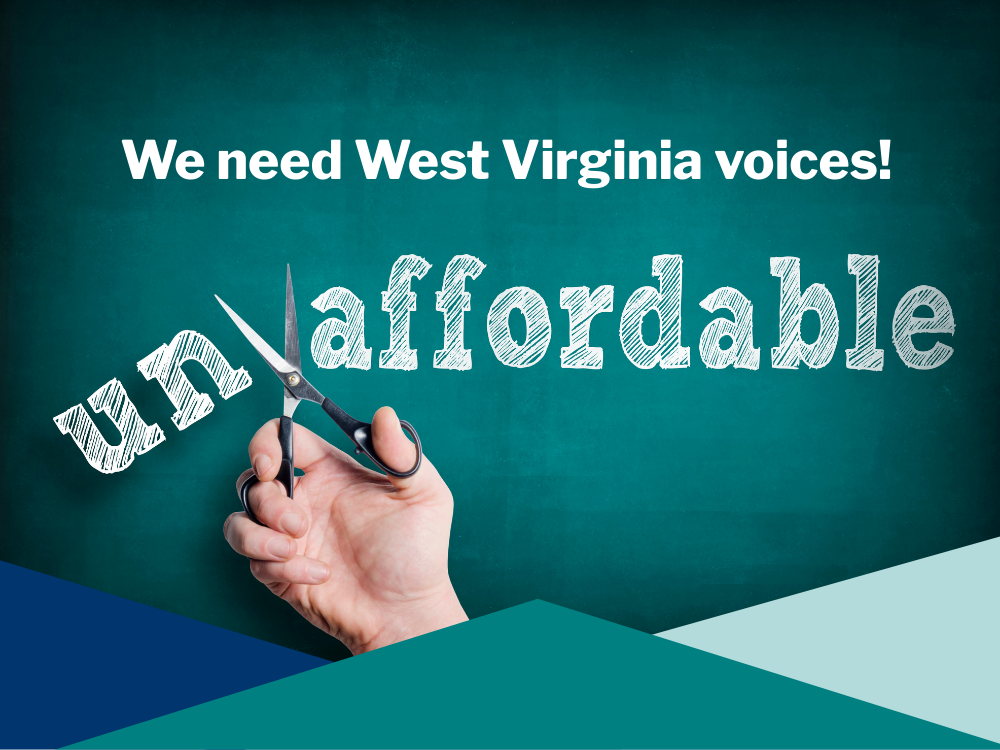
We are in need of healthcare stories: West Virginians willing to share struggles to afford medications or care, success stories due to gaining Medicaid coverage, and most important to us right now are stories of claim denials, especially from the Medicaid MCO Aetna Better Health of West Virginia.
Stories are how we educate the public, and policymakers. Stories are how we fight for change.
Share Your Healthcare Story
We need claim denial stories, especially of Medicaid insurer Aetna Better Health of WV.
Help us find stories, champion these people’s cases, and fight their denials on their behalf by shedding light on them, making their struggles public, and bringing these cases to Aetna.
Here’s how you can share your stories, and afterwards we’ll reach out to schedule a follow-up conversation.
- Story collection form: www.hcstorieswv.org
- Video submissions: http://ppls.ac/aetnawv
- Email careovercost@wvcag.org
- Leave us a voice message at (304) 346-5891
But you may be asking “Why Aetna?” Well, it’s because Aetna Better Health of WV is denying and delaying healthcare to West Virginians, healthcare that should be covered, and it looks like they are doing this because it’s profitable. People are going bankrupt from medical debt, or staying sick, even dying, so that Aetnqa can squeeze out more profits.
Aetna isn’t the only one. They are part of the private health insurance industry, whose business model relies on denying members the treatments and medicines they deserve. Insurance companies make a lot of money off of denying our claims, to the tune of $260 Billion annually. Nearly 1 in 5 claims are denied (17%), and only about 0.2% of claims are appealed. In other words, since most people can’t figure out the complicated appeals process, it is a near guarantee that companies get to keep that money instead of paying it out for people’s health care.
Claims denials are when a health insurance corporation refuses to pay for care that your doctor prescribed and you’ve already received – sticking you with the bill, unnecessary medical debt and even bankruptcy. A prior-authorization denial is when your insurance refuses to pay for a medicine, surgery or other treatment before you even get it. So you can’t get the care you need and stay sick, stay injured, or even die as a result. These denials hurt black and brown folks (especially women and infants), and rural and poor folks the hardest.
Private insurance companies deny well over 248 million claims or pre-authorization requests from their policyholders annually, often using AI.
Aetna Better Health of WV, according to a July DHHS report, has a prior authorization denial rate of 13.7%. And their medical directors, according o a CNN article, don’t read patient’s records before denying claims, they don’t have enough time to because they are given ridiculously small windows for reviewing each case. In addition, in Oklahoma, a patient was awarded a $25 million dollar verdict in a “bad faith” case after Aetna company denied cancer treatment.
Aetna, according to Fierce Health, had record revenues of $91.4 Billion in 2022, up 11% over the previous year.
Aetna’s parent corporation, CVS Health:
- Paid their CEO Karen Lynch $21,317,055 last year.
- Took $6 billion in profit from their Aetna insurance division in 2022 alone.
- Spent $20.57 million on lobbying in the 2021-2022 cycle.
Where are Aetna’s huge profits coming from? They are a direct result of the denials of care to sick patients.
My roommate has continually been denied his claim for hernia surgery and it’s as big as a head of cabbage at this point. Why? Because it’s apparently “not life threatening”. I spoke with a lady who’s doctor’s request for a CT Scan took months and months to finally be approved after multiple appeals, but by then, her cancer had spread. Other people have had claims denied after they’ve seen the doctor, with little explanation as to why, and now they are afraid to see their doctor because of the fear of more unexpected debt.
They are not alone. Nearly 1 in 5 people have a claim denial story. But people are afraid to speak up. We need your help to encourage them to raise their voices and share their truth. Enough voices raised can be deafening, and too loud for lawmakers to ignore, especially a big election year coming up.
On Wednesday, October 11th, at around lunchtime, WV Citizen Action Group, People’s Action, WV Poor People’s Campaign, Rise Up WV, New Economy Works WV and others held a demonstration and press conference outside of the Medicaid MCO Aetna Better Health of WV’s offices, located at 500 Virginia St. East, Charleston, WV 25311. Our demand was and is that health insurance corporations stop denying care to its members to pad their profits, honor their contractual obligation, do their job to provide coverage, stop profiteering off of our care, and instead put Care Over Cost.
This event was one of 14 that happened nationally led by the Care Over Cost campaign.
Before the demonstration, we spoke with the people inside, respectfully, and they agreed to meet with us in the coming months. But, only if we have claim denials to bring to them.
Please lend a hand. Share your story. Ask people you know to share theirs. Help us connect with those harmed by the healthcare industry, hear these stories and bring them to light, and for Aetna, directly to them for our next in-person meeting.
Help us fight on on the behalf of West Virginians unable to get the care they need, or are in overwhelming debt. Let’s honor them by sharing their stories and fighting for change.